Cervicogenic Dizziness – the data needs more data!
One of my favorite excerpts from an editorial in quite awhile…
Clinicians should quit looking for overly simplistic answers. Clinical diagnosis, like producing a great wine, is complex and requires an appreciation of the data that can be gathered within the nuances of patient interaction
I do not think I am alone when we all learned clinical tests, or special tests, in PT school, it was one of the coolest things ever! It was gratifying to go from theory to “practice” and actually be able to diagnose something! Unfortunately, as I continued to learn more, this bubbled busted—and busted with explosive power.
ARE YOUR DIZZY AND NECK PATIENTS GETTING STUCK AT BEING 75% BETTER? WE CAN HELP.
If only it was that easy.

The recent editorial, entitled “Orthopaedic special tests and diagnostic accuracy studies: house wine served in very cheap containers” in BJSM by Hegedus/Wright/Cook (free to access) brings to light the errors associated with clinical diagnostic tests with overall intention of clinicians to utilize clinical reasoning on refined data.
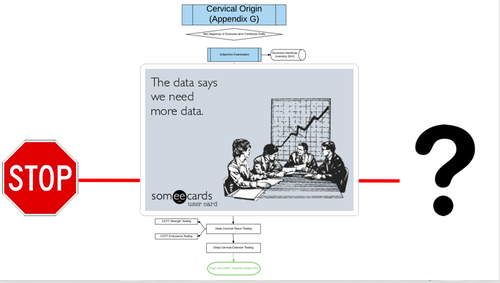
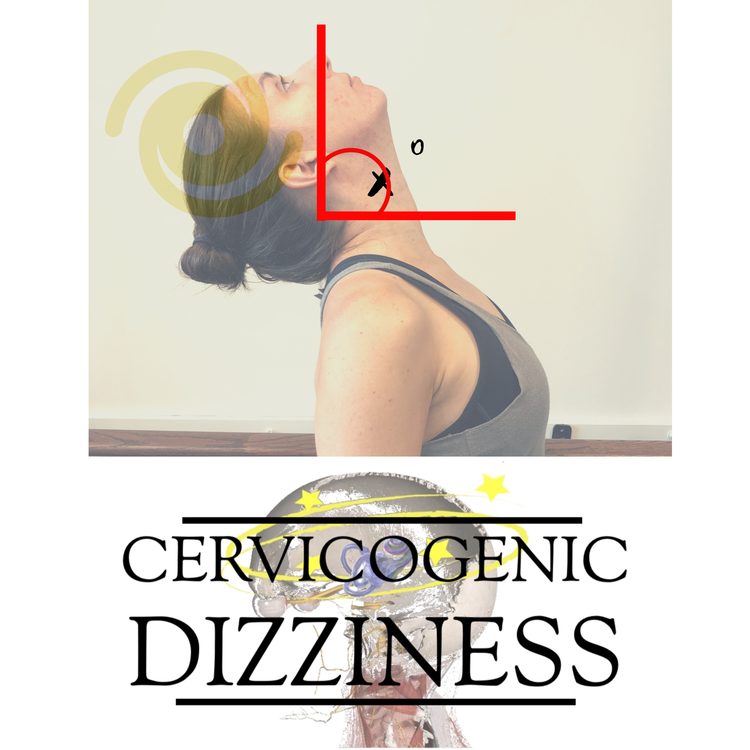
We have these special tests for cervical vertigo / cervicogenic dizziness–i.e. joint position error testing and cervical torsion tests, to aid in our hypothesis—but unfortunately, just like diagnostic tests to rule in hip/shoulder impingement and meniscal tears–these are limited.
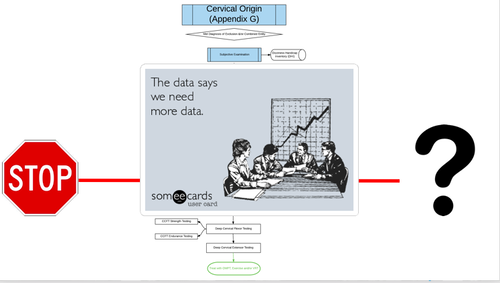
So when you ask someone about the diagnosis of Cervicogenic Dizziness—back away if he/she quickly throws at you Joint Position Error Testing—even though this is promising, we are better than that. We should be better than that. JPE testing will simply add more data to the already established data. The already established data is a stronger foundation, a safer foundation, for your clinical examination.
I have spent the last few years of my clinical career examining every article published (in multiple languages!) coupled with clinical practice to provide the most optimal diagnostic process to put together my Optimal Sequence Algorithm. In my personal opinion, I think this diagnosis is the most controversial (besides SIJ!), but ultimately takes the gold medal in clinical reasoning due to the often, and intimidating, nature of dizziness in non-benign conditions, including vascular and other central disorders. No one should be comfortable jumping into the upper neck with someone experiencing dizziness without sound judgement and training.
As previously quoted, “clinicians should stop looking for overly simplistic answers”. Let me help guide your thought process in this unnerving and overwhelming part of the human body. These patients are walking in your door—let me help you get them better.
Cervicogenic Dizziness Course
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the authors (husband–a manual therapist a wife—a vestibular specialist), teach a very unique course combining both the theory and practice of vestibular and manual principles in their 2-day course. Pertinent to this blog post, the 2nd day includes the “Physio Blend”, a multi-faceted physiotherapist approach to the management of Cervicogenic Dizziness, which includes treatments of the articular and non-articular system of manual therapy and the most updated sensorimotor exercise regimen.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for more information.
AUTHORS
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts