It is now well know the correlation between symptoms and physiological effects that are sustained following patients who suffered from concussion and whiplash. Even though there are still apparent differences clinically, we can now feel comfortable to lump these two conditions together. It may surprise some readers --- but in this article -- and most likely in the medical literature in the future -- we will collectively call the injury a mild traumatic brain injury (mTBI).

Galea and colleagues just came out with a Meta-Analysis in 2018 to determine whether persistence of sensorimotor or physiological impairment exists between 4 weeks to 6 months post injury. More than likely the clinicians reading this article will see a patient suffering from symptoms > 10 days following the injury for definition of post-mTBI symptoms, but could be between 4-12 weeks so your patient fits in nicely in the objective. More than likely we are seeing them for dizziness, headaches, neck pain, difficulty concentrating, etc.
For those interested in reading the entire analysis, feel free to reach out to me for article, but for blog purposes; here is the conclusion:
Findings demonstrate that persistence of sensorimotor and physiological changes beyond expected recovery times following subacute mTBI in an adult population is possible. These findings have implications for post-injury assessment and management.
BIG POINTS I WANT TO YOU TO GET OUT OF THIS CONCLUSION.
Firstly, the "is possible" statement from first glance isn't conclusive at all---but for a meta-analysis---I will take it!
Secondly, and reason we aim for to read and perform research, is this statement, "these findings have implications for post-injury assessment and management".

The assessment and management of this very complicated and the challenging condition of mTBI is beyond what can be written in words. In fact, my wife and I teach 16 HOURS worth of updated and modern content to make you more confident in treating someone suffering from mTBI who has Cervicogenic Dizziness / Cervical Vertigo. This doesn't even include the science and application of treating the other symptoms!
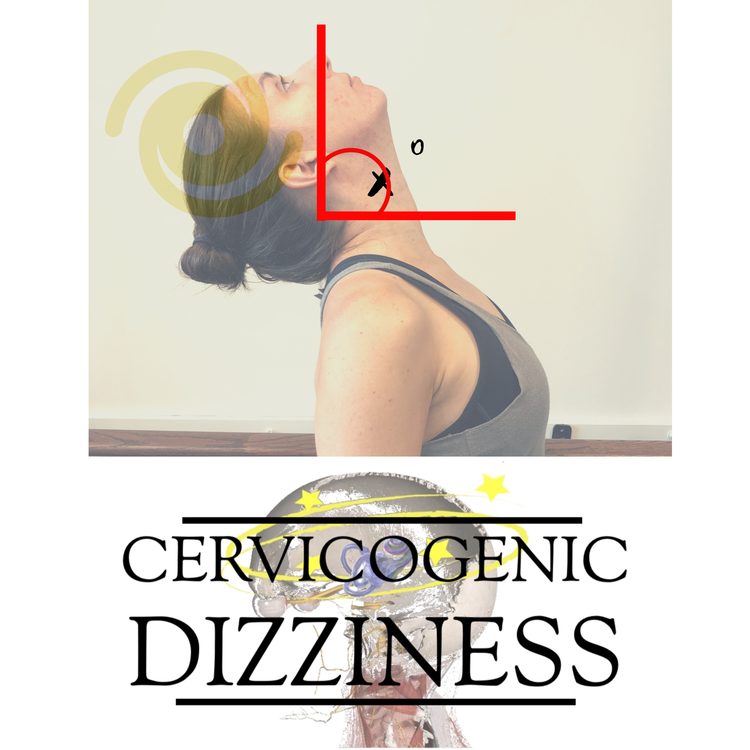
We do know that the presentation of a patient who could have Cervicogenic Dizziness / Cervical Vertigo is much more than someone who has suffered a recent mTBI; but this Meta-Analysis has huge implications for our instructional content and approach. In fact, a large percentage of our course is dedicated to the assessment and management of Sensorimotor changes.
DOESN'T THIS LAST BOLDED STATEMENT CORRELATE NICELY WITH THE LATEST HIGHEST-LEVEL EVIDENCE FROM GALEA ET AL THAT WAS QUOTED ABOVE?
Cervicogenic Dizziness Course
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the authors (husband–a manual therapist a wife—a vestibular specialist), teach a very unique course combining both the theory and practice of vestibular and manual principles in their 2-day course. Pertinent to this blog post, the 2nd day includes the “Physio Blend”, a multi-faceted physiotherapist approach to the management of Cervicogenic Dizziness, which includes treatments of the articular and non-articular system of manual therapy and the most updated sensorimotor exercise regimen.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for more information.
AUTHORS
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts