Why do some BPPV patients require more repositioning procedures for relief?
Treatment of BPPV can be one of the most rewarding procedures in the field of physical therapy --- both for the patient but also the clinician! There are not many instances in our profession that we can make life changing results in just one visit!

When the diagnosis of posterior canal BPPV (most common canal involved) is made through history taking and clinical examination, the application of canalith repositioning procedure can be effectively performed with success rate as high as 80%. However, for some individuals, repeated manuevers are necessary to achieve results.
The question is, why?
This has been studied over the years with conflicting results over factors including:
- Age
- Which canal is involved
- Duration of symptoms
- Intensity of symptoms and
- Comorbidities (diabetes, high blood pressure, migraines, etc)
For most vestibular therapists, the application of two canalith repositioning manuevers are performed in the same day. If the second diagnostic test (i.e. Dix-Hallpike) is negative, we can be more confident of best results as the Epley Manuever (or comparable procedure for a different canal) was successful. We would reach out to say this is a fair assessment of a typical treatment regimen.
So, for those requiring more than one or two procedures-- the question remains --- is the issue in a different canal, is the issue due to chronicity of symptoms, is the issue due to age, etc etc?
I want to invite you to Korkmaz & Korkmaz's retrospective study in 2015, entitled, "Cases requiring increased number of repositioning maneuvers in benign paroxysmal positional vertigo".
These authors studied this exact question, and found the following conclusion:
Our study showed that patients with hypertension required higher number of treatment visits compared to patients with no hypertension....The presence of hypertension is a risk factor for repeated maneuvers in BPPV treatment. When dealing with patients with hypertension, physicians must be aware of the high probability of repeated treatment sessions.
So for us in rehabilitation medicine, we of course cannot diagnose hypertension NOR treat it via pharmacological methods....so you may ask, okay...I see this day to day in the clinic but what can I DO about it.

We all know hypertension is a major vascular condition and can obviously hinder blood perfusion through the arterial system, especially smaller vessels inserting into the vestibular organs. Some clinicians express that the ischemia from hypertension may cause more extensive otolithic debris formation than usual and that may be why multiple maneuvers are needed to reposition the otolithic particles in these group of patients.
To go outside of the physical therapy, even chiropractic and osteopathic literature, as well-rounded clinicians, we should enter the information from the acupuncture works. The use of acupuncture has been used for chronic dizziness for over three thousand years (vs PT Epley Manuever starting in 1983, Chiropractic in 1890s & Osteopathic in 1870s). The point of this post is not to delve into the practice of acupuncture, but to simply educate others in our profession of other potential treatments and why.
The mechanisms behind traditional acupuncture is WAY beyond the means of this post (and not the point as not my speciality), but for the most part, we can capture that increased blood flow and circulation (alleviate insufficiency potentially caused by hypertension) in the vertebral - basilar artery (and subsequently downstream to vestibular organs) is a MAJOR pathogenesis mechanism of results following acupuncture for dizziness.

So, if for thousands of years, the treatment of dizziness can be attributed to blood flow and circulation---treated with acupuncture and other methods---and the recent work of Korkmaz & Korkmaz showing the highest risk factor for more treatments to improve same diagnosis is hypertension --- why would it not be plausible to combine manual therapies to the cervical spine IN ADDITION TO canalith repositioning procedures (which is accompanied by treatment clinical guidelines) to potentially reduce number of repositioning procedures and get faster results?
If you think along these concepts, and add that the #1 comorbidity in Korkmaz & Korkmaz's study is spine problems (over 1/3 of patients!) --- how could you think that is is not feasible to combine both manual therapies (to the cervical spine) and vestibular therapies for the most effective treatment of BPPV?
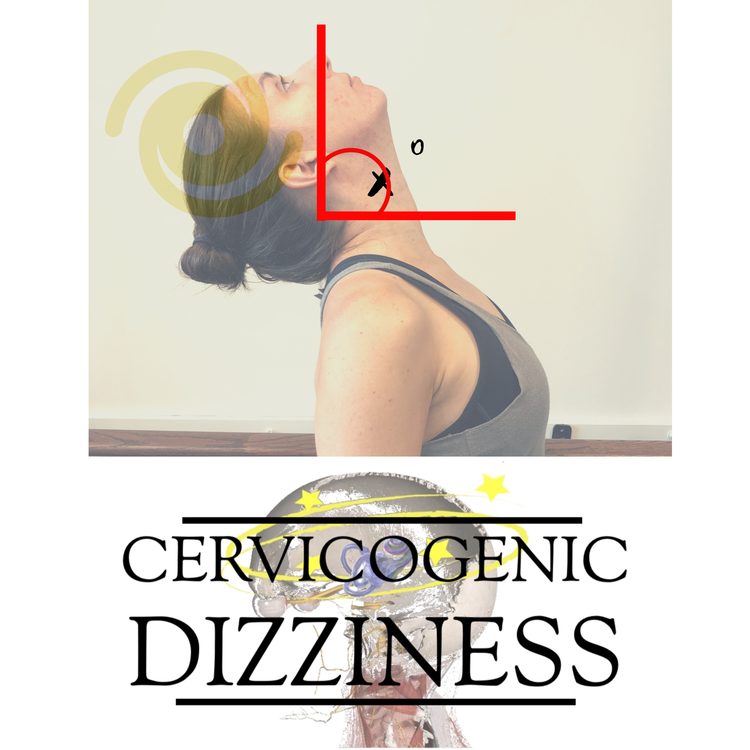
This is WHY we bring in the best of the best in manual therapies and vestibular therapies for those suffering from dizziness. Let's not even call it Cervicogenic Dizziness --- but simply Dizziness.
You will not get the combination of manual therapy, vestibular and sensorimotor training anywhere else! Learn more how to get the best results in your patients!
Stay tuned to future blog describing evidence for increased blood flow and circulation following manual therapies.
Cervicogenic Dizziness Course
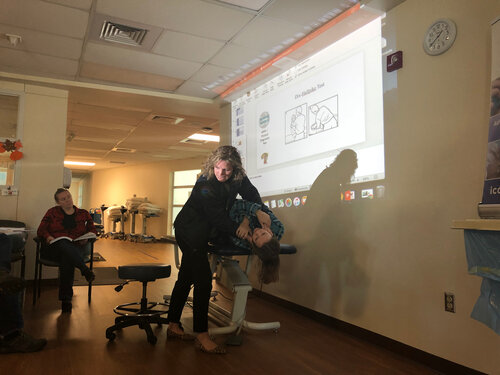
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the authors (husband–a manual therapist a wife—a vestibular specialist), teach a very unique course combining both the theory and practice of vestibular and manual principles in their 2-day course. Pertinent to this blog post, the 2nd day includes the “Physio Blend”, a multi-faceted physiotherapist approach to the management of Cervicogenic Dizziness, which includes treatments of the articular and non-articular system of manual therapy and the most updated sensorimotor exercise regimen.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for more information.
AUTHORS
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts