When most physical therapists think of peripheral vestibular deficits, we typically think of isolation of a condition, such as BPPV. This, at least since 1926, involves canalith repositioning testing via Dix-Hallpike manuever and treatment, since early 1980s, with Epley Manuever.
A large and sometimes missing link is that individuals with unilateral peripheral vestibular deficits acutely constrain their head movements relative to their trunk to reduce symptoms of oscillopsia, dizziness and nausea. These altered movement patterns can result in the loss of normal decoupling of head motion from trunk motion while walking and potentially have a less efficient gait pattern and postural activity tolerance.
For the therapists who work in inpatient, home health setting and even outpatient rehabilitation centers, we typically examine dynamic gait tasks and even though not as high priority of movement patterns to a generalist assessment, these movements significantly impact head and trunk requirements. As you can see from Table 1 below from Paul et al 2017 paper, entitled "Characterization of Head-Trunk Coordination Deficits After Unilateral Vestibular Hypofunction Using Wearing Sensors", the Functional Gait Assessment, Timed Up & Go Test and 2-minute Walk Test have large influence of head and trunk rotation influences.
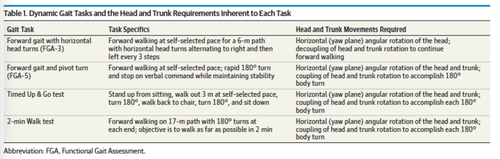
Table from Muhammed et al 2019 Post-treatment NDI was significantly lower in Group C compared to the other two groups (p<0.001) and was comparable in groups A and B (p=1.000). The percentage drop of NDI was significantly higher in Group C compared to the other two groups (p<0.874), but the magnitude of NDI drop was comparable between Groups A and B (p=1.000, Table 2).
Paul et al 2017
Even though this study examined deficits in gaze and postural stability of the head and trunk after surgically induced unilateral peripheral vestibular hypofunction, the physical therapist can relate the head and trunk movements required for any peripheral vestibular disorder and relate the impact of the cervical proprioceptive system in active movement of the head and trunk coupling moments.

You can see in the 3rd column on right above that yaw plane (angular rotation) of the head and trunk that relates to coupling of head and trunk rotation is necessary to accomplish these tasks. Considering C1-2 (Atlanto-Axial Joint) is 50% of rotation of the cervical spine, this could be a significant limiting factor in your patient. Read a previous post on how this joint restriction relates to Cervicogenic Dizziness.
Paul et al 2017 concluded,
A key component to recovery from peripheral vestibular deficits is the regular exposure of head movements that may induce gaze and postural stability errors and therefore facilitate recovery.
If you are a trying to implement regular exposure of head movements but run into a wall of neck pain, restriction of range of motion or even lightheadiness associated with these movements, then our class of diagnosing and treating Cervicogenic Dizziness can be of benefit to you. Most of our classmates think this class is mostly for post-concussive or whiplash patients; but I disagree that it can be even more important in reducing fall risk and improving movement patterns in the elderly! The association of cervical disc disease and restriction in mobility of the cervical spine is by far more prevalent in society that trauma-based cervical conditions.

As Paul's study arose in the literary works, another fantastic investigation by Julia Treleaven & colleagues out of Australia in 2018 suggests that neck pain subjects have difficulty moving their trunk independently of their head. Her work on altered trunk head co-ordination in those with persistent neck pain indicates that tasks are performed more slowly with neck pain patients, which directly correlates to the speed and accuracy testing of gait testing through Functional Gait Assessment, 2-minute Walk Test and Timed Up and Go Test.
Even if you are not treating "dizziness or vertigo", but are involved in reducing fall risk in patients in any setting, contact us to see if this course can help your patients. As you know, the Home Health Physical Therapy industry is performing Vestibular Rehabilitation and continues to focus on Fall Risk Reduction. A missing link of improving postural control and balance can be limitation to the upper cervical spine. Specific diagnostic and treatment approaches are available to benefit your patients and continue to raise the bar of rehabilitation.
Cervicogenic Dizziness Course
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the authors (husband–a manual therapist a wife—a vestibular specialist), teach a very unique course combining both the theory and practice of vestibular and manual principles in their 2-day course. Pertinent to this blog post, the 2nd day includes the “Physio Blend”, a multi-faceted physiotherapist approach to the management of Cervicogenic Dizziness, which includes treatments of the articular and non-articular system of manual therapy and the most updated sensorimotor exercise regimen.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for more information.
AUTHORS
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts