One of our jobs as physical therapist's include identifying red flags and ruling out more serious disorders that warrant referring out.

Considering I treat a great deal of spinal patients (especially ones of increasing age), one disorder that comes to mind is identifying cervical spine myelopathy (CSM). The main concern with this condition is the compression placed on the actual spinal cord, not nerve roots. If neurological status is worsening, this would mean immediate referral. There are many sites to read about the pathophysiology further, but here is one you can go to.
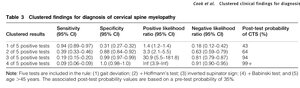
In 2010, Cook et al published a paper entitled, "Clustered Clinical Findings for Diagnosis of Cervical Spine Myelopathy". The findings provided a clinical decision making tool that had high sensitivity (to rule-out CSM) and even high specificity (to rule-in CSM). The picture below shows these values:
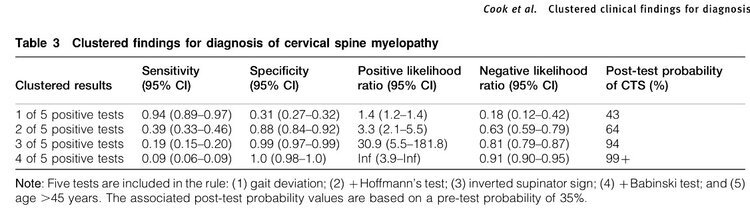
Out of the five tests, the two that students have the most trouble with (and never see a positive sign) are the Hoffman's Test and Inverted Supinator Sign. I find both of these to have high specificity values in my practice (which means if the test is positive, a high probability of an upper motor neuron disorder is present). So, here they are:
Hoffmans' Test:
How to perform: Grasp the patient's middle phalanx of 3rd digit at distal end with your 2nd and 3rd distal phalanges. Flick the patient's distal phalanx into flexion using your thumb.
Positive test: Adduction of thumb and/or flexion of fingers
A positive test or abnormal response provided by my YouTube Page:
Inverted Supinator Sign
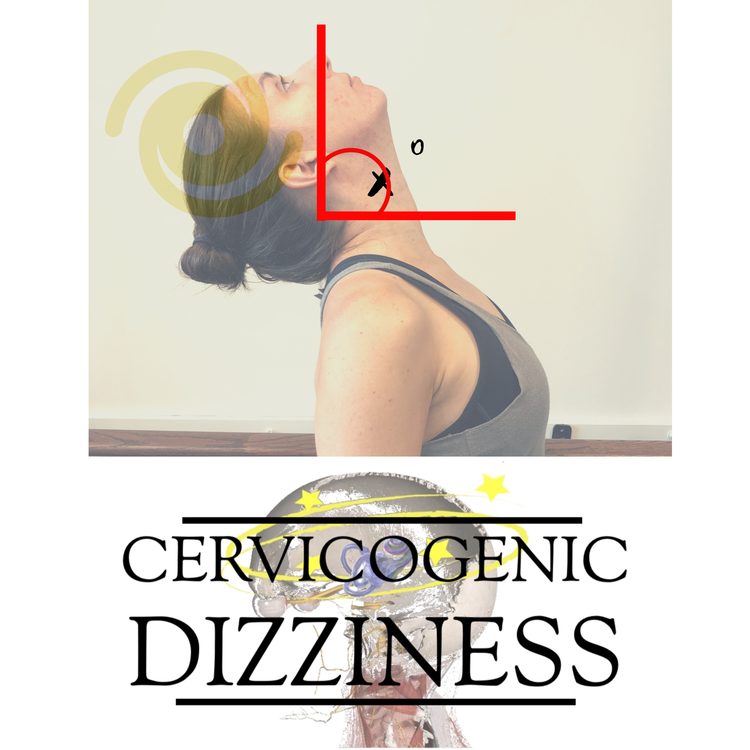
How to perform: Using reflex hammer, strike the brachioradialis tendon near radial styloid process at distal end of radius (C6 DTR).
Positive test: Finger flexion
A positive test or abnormal response provided by my YouTube Page:
We definitely recommend screening for cervical myelopathy prior to cervical manipulation procedures or quite frankly, simply as a neurological screening tool prior to any type of therapeutic intervention. This CPR tool gives us a solid ruling-in and ruling-out process that can help clinicians be confident about what is underlying the skin in patients with unsteadiness, dizziness, neck pain and headaches. We teach this approach for our Cervical Dizziness Course to make sure dizziness and unsteadiness is not due to myelopathic symptoms.
Cervicogenic Dizziness Course
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the authors (husband–a manual therapist a wife—a vestibular specialist), teach a very unique course combining both the theory and practice of vestibular and manual principles in their 2-day course. Pertinent to this blog post, the 2nd day includes the “Physio Blend”, a multi-faceted physiotherapist approach to the management of Cervicogenic Dizziness, which includes treatments of the articular and non-articular system of manual therapy and the most updated sensorimotor exercise regimen.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for more information.
AUTHORS
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts