Impaired Sensorimotor Outcome Measures for Clinicians
Impaired Sensorimotor Outcome Measures for Clinicians
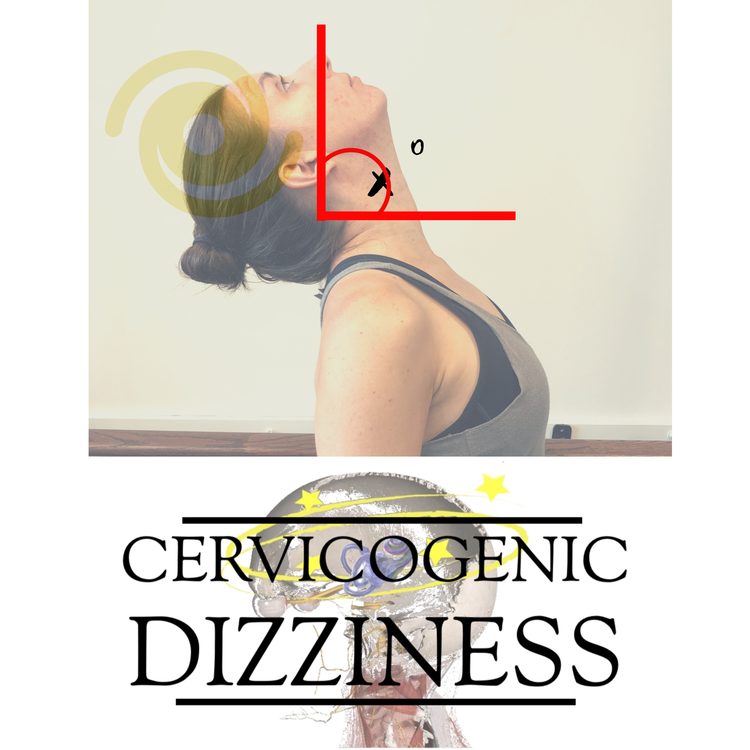
Sensorimotor processes are vital for maintaining stability and controlling movements of the head. Proprioception is typically the most important component of sensorimotor control and is tested clinically in the cervical spine with the joint position error test. This is generally assessed by measuring repositioning errors when subjects attempt to reproduce specific head positions, and in such tests, subjects are normally blindfolded to remove visual cues.

The importance of proprioception in the control of movement suggests that any impairment of position or movement sense may have adverse effects on motor control mechanisms, leading to an increased risk of injury. This is often seen in individuals following a traumatic cervical spine event (such as whiplash or concussion), but also in individuals with non-specific cervical spine pain. It is often tested in patients with potential diagnosis of Cervicogenic Dizziness.
For those who utilize the joint position error test and the targets to improve motor control know the limitations behind this procedure in full symptom resolution of someone who has Cervicogenic Dizziness. One of the biggest false-negatives I see is the response to training, which can improve just within a session by performing the same task repeatedly. This is why the latest research recommends testing rotation and extension 6 times to determine if truly a deficit!
Therefore, I recommend utilizing subjective, impairment specific outcome measures, in addition to objective tests (i.e. Joint Position Error Testing) to not only determine change in your therapeutic interventions, but also to tease out any remaining symptoms that the patient expresses on paper, but not in front of the clinician and is clinically a low-threshold symptom that doesn't appear on objective tests.

Here are the top 3 Sensorimotor Outcome Measures that you can utilize in the clinic:
1. DIZZINESS HANDICAP INVENTORY (DHI)
The Dizziness Handicap Inventory (DHI) is a validated, self-reported questionnaire, which is widely used to evaluate the functional, emotional, and physical impact of dizziness in patients’ daily life. It consists of 25 questions about daily problems associated with dizziness, and each question is given a score of 0, 2, or 4. It has been shown to be a highly reliable and responsive tool.
A score of 0 means that the condition described in the question never happens, 2 means it sometimes happens, and 4 means it always happens. Following a study by Whitney et al 2004. the DHI scores are graded as mild (0 to 30 points), moderate (31 to 60 points), and severe (61 to 100 points). A change of more than 10% in a patient’s DHI score demonstrates a clinically significant change over time, and a change of 18 points is considered a true change (Treleaven 2006, Tamber & Wilhelmsen et al 2009).
The Dizziness Handicap Inventory has also been described previously by Susan Reid and colleagues as a diagnostic screening tool to rule in or rule out Cervicogenic Dizziness.
You can download a copy of the DHI here.
2. VISUAL COMPLAINT INDEX
The Visual Complaint Index consists of 16 visual symptoms with options to rate frequency and severity on 3 and 4 point rating scales, respectively (Treleaven and Takasaki 2014).
Scores for each item are then multiplied and added overall to achieve a score out of 164. A mean score of 27.4 previously identified in individuals with neck pain (Treleaven and Takasaki 2014) was used to identify clinically relevant vision related complaints.
Symptoms suggesting to be associated with neck pain are more vision related items vs vision specific items. The following lists the most prevalent to least prevalent in patients with neck pain (Hülse and Holzl, 2000, Kristjansson and Treleaven, 2009, Treleaven and Takasaki 2014):
‘Needing to concentrate to read’ (most troublesome and prevalent with neck pain)
‘Blurred vision’ (more specific to whiplash injuries and high levels of pain/dizziness than general neck pain)
‘Words or objects moving’ (more specific to whiplash injuries and high levels of pain/dizziness than general neck pain)
‘Difficulty judging distances’ (more specific to whiplash injuries and high levels of pain/dizziness than general neck pain)
‘Visual fatigue’
'Sensitivity to light'
'Eye Strain'
'Heavy Eyes'
Even though the Visual Complaint Index has not been used specifically in the literature for individuals who suffer from Cervicogenic Dizziness, it can be a useful tool for those who treat patients following whiplash, concussion and mTBI injuries to assist in clinical reasoning behind treating the cervical spine in addition to oculomotor and vestibular rehabilitation. We recommend utilizing the scale provided below and compare to symptoms provided and objective evaluation above to determine if appropriate to refer out for cervical treatment or even perform yourself.
You can download a copy of the Visual Complaint Index here
3. SPACE AND MOTION DISCOMFORT
“Space and motion discomfort” (SMD) describes dizziness that is provoked by visually provocative situations (i.e. grocery stores, malls, ceiling fans). The Space and Motion Discomfort II (SMD II) scale is a 9-item index of space and motion discomfort (Jacob et al., 1993). In relation to Cervicogenic Dizziness, muscle guarding and limitation in range of motion from altered space and motion discomfort can lead to cervical symptoms associated from disuse. This is one reason for kinesthetic awareness deficit.
The association between SMD and abnormal balance has been shown to be specific for somatosensory dependence (Jacob et al 2016). Scores for each item (0–3 rating scale) are multiplied by a factor of 10 and summed for cumulative score. A mean total score of 82.4/270 previously recorded in a vestibular population (Jacob et al., 1993) was the nominated clinically relevant threshold.
To date, there are no specific studies utilizing the SMD II with Cervicogenic Dizziness, however, the following visual symptoms included in the index and associated reasons for potential cervical involvement are listed below:
Looking up at tall buildings. Cervical extension is the most disturbing positional movement associated with Cervicogenic Dizziness.
Leaning far back in chair. Cervical extension (if leaning back involves mostly upper cervical extension vs fluid cervical extension and then upper cervical extension) is the most disturbing positional movement associated with Cervicogenic Dizziness.
Discomfort increase during the day. Muscular fatigue and disturbance in endurance, especially if in sitting positions all day, are a contributing factor to altered muscular capacity and a symptom of Cervicogenic Dizziness.
You can download a copy of the Space and Motion Discomfort (SMD II) scale here
If you feel your patient is having Sensorimotor disturbances and/or symptoms associated with neck pain, we recommend getting subjective reporting via the above outcome measures. There are many more in the literature as well but these are the top 3 for Sensorimotor implications.
The treatment of Cervicogenic Dizziness has historically been viewed within a manual therapy construct, but knowing the limitations behind long-term effects of manual therapy and double entity component of dizziness symptoms, we teach specific Sensorimotor exercises for this population. We find the combination of manual therapy and sensorimotor exercise (not just stretching/strengthening of neck muscles and vestibular rehabilitation) gives the most well-rounded and optimal results for your patients with Cervicogenic Dizziness.
Cervicogenic Dizziness Course
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the authors (husband–a manual therapist a wife—a vestibular specialist), teach a very unique course combining both the theory and practice of vestibular and manual principles in their 2-day course. Pertinent to this blog post, the 2nd day includes the “Physio Blend”, a multi-faceted physiotherapist approach to the management of Cervicogenic Dizziness, which includes treatments of the articular and non-articular system of manual therapy and the most updated sensorimotor exercise regimen.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for more information.
AUTHORS
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts