Suspecting a patient has VBI? You could recommend this.
The probability of a patient arriving to your outpatient, physical therapy office with symptoms associated with vertebrobasilar insufficiency (VBI) is very, very, very minimal. VBI is an important diagnosis to consider, as many symptoms can mimic benign peripheral etiologies in our industry.
Most of the data in the physical therapy world on the incidence of VBI is after a manipulation, which is anywhere 1 in 20,000 to 1 in 1 million. But I'm not talking about iatrogenic causes, but actual spontaneous events, which is what would most likely lead someone to come into your office.

The probability of this non-benign condition is higher if you treat neck pain and even higher if you treat headaches and dizziness. We know the work by Lucy Thomas especially has shown in chart reviews that dizziness, headaches and balance/postural issues are high impact symptoms of VBI. Her recent work has confirmed the previous work by Alan Taylor & Roger Kerry from mid-2000s.
As differential diagnosis machines, we need to be to be able to effectively address neuromusculoskeletal conditions. Clinicians should always have VBI as a small nugget in the back of the head as quite frankly, a central cause of headaches, neck pain or dizziness is not one of which we should back down lightly in our knowledge of differential diagnosis.

We have written in the past (here, here, and here) about ruling out vascular sources that leads to these symptoms in the past and even have written about the use of the HINTS examination to assist clinicians in differentiating between central and peripheral causes of dizziness. There has been a significant spike of power behind simply looking at blood pressure and we know these tools are highly necessary before doing any type of mechanical testing, such as the VBI test.
Another tool that is not spoken much about, but we have in our algorithm to rule out spontaneous disorders, is the use of biomarkers. The use of biomarkers for differential diagnosis is used for other conditions (such as temperature for a fever) but not spoken of much in the physical therapy world.
The use of blood biomarkers for differential of VBI was spoken of over 20 yrs ago quite but to my readings of the literature in the past decade, I haven't seen much about it until now. A recent study in 2020 out of South Korea by Sohn et al brought this information back to life and I want to share with you all.
The authors looked at blood biomarkers to examine differential diagnosis in 2 groups --- 1 is central vertigo (CV) and 2 is peripheral vertigo (PV). We know VBI would be under central vertigo. The patient also went under full neurology examination including having MRA and CT scan.
Here is what they found:
Serum NSE and S100β levels are significantly higher in patients with CV, such as occurs with posterior circulation ischemic stroke or vertebrobasilar insufficiency. S100β and NSE may serve as serum biomarkers for differentiating between CV and PV in patients with acute-onset vertigo.
TAKE HOME POINTS
First, I take this information as another recommendation I could make to the medical staff to obtain, in addition to full neuro examination including MRA, if I suspect central vertigo through my clinical examination.
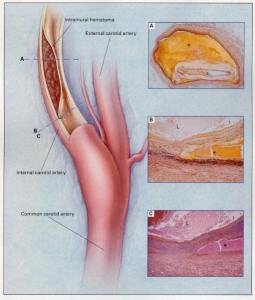
Secondly, I take this information as another non-mechanical test (such as prior to cervical ROM and VBI testing) that could be achieved before placing undue stress on the blood vessels that could take a spontaneous dissection to a full dissection. We all know how this is usual what happens and what has given manipulation such a bad name in the past. We had a great article we wrote awhile ago about this happening NOT from manipulation, but from cupping and massage. I think this can help you understand this concept more.
Thirdly, I know we can't order or have ability to obtain blood biomarkers, nor understand how to read the results professionally. Therefore, I take this type of study as a physical therapist with confirming the already established Optimal Sequence Algorithm for diagnosing not only Cervicogenic Dizziness, but for Cervical Artery Dysfunction.
Cervicogenic Dizziness Course
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the authors (husband–a manual therapist a wife—a vestibular specialist), teach a very unique course combining both the theory and practice of vestibular and manual principles in their 2-day course. Pertinent to this blog post, the 2nd day includes the “Physio Blend”, a multi-faceted physiotherapist approach to the management of Cervicogenic Dizziness, which includes treatments of the articular and non-articular system of manual therapy and the most updated sensorimotor exercise regimen.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for more information.
AUTHORS
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts