Cervicogenic Dizziness – Controversial Entity between Professions
There is controversy between professions.
Gonzalez and Palacios in 2001 wrote an article, “Cervical Dizziness: A Scientific Controversy” in Fisiotherapia Journal. The final wording in the manuscript, albeit translated from Spanish to English, basically sums of the controversy that surrounds the diagnosis and treatment of cervicogenic dizziness in one sentence.
For practitioners of physiotherapy and manual medicine, the vertigo of cervical origin is almost unquestioned, treatable and solvable entity mostly, while for professionals otolaryngology and scholars of the vestibular apparatus and balance, their relationship remains hypothetical and in many cases questionable.
Gonzales and Palacios 2001
There is controversy between professions.

To those in the professions of manual medicine and rehab—osteopathy, acupuncture, chiropractic and physical therapy—the diagnosis and treatment of cervicogenic dizziness obviously occurs and can be present in many subsets of different populations. To anyone who has dealt with this in their office, this seems to be a no brainer as results speak for themselves. However, outside the manual medicines, including otoneurology and audiology; the diagnosis of exclusion stands concrete and likelihood of referring out is much less likely. In fact, most of the literature denotes less than a 10% prevalence rate with dizziness from cervical origin and majority of studies consistently outside of the rehabilitation and manual realm do not list it at all under differential diagnosis.
Could cervicogenic dizziness be embellished in the manual medicine fields and neglected in the allopathic medical field?
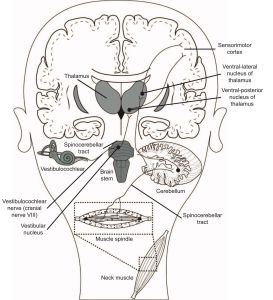
Picture from: Cheever et al 2016
The question remains, what makes the incidence and prevalence so different between the professions?
Is it a business argument? Obviously manual medicine and rehab can benefit from treating these patients, where medication and imaging does not work.
Is it science? The diagnosis of dizziness from a cervical origin continues to be under debate and scrutinized (Brandt 1996, Brandt/Bronstein 2001). There is a discrepancy in the pathophysiology, lack of diagnostic criteria including a well established clinical test or a specific laboratory test, and many other diagnoses can be a convincing alternative reason for symptoms.
Is it ethical? With a lack of a true diagnostic test, unknown epidemiological data points and prognostic time line of improvement—could the manual medicine fields provide unethical treatments— scientific implausible treatments or even fraud?
Is it training? Anyone in the physical therapy field knows the lack of training in the MSK field by physicians—we fuss about this all of the time. We contend about their lack of knowledge to refer to us for even less controversial diagnoses. You can imagine, considering even a small percentage of manual medicine that focuses on cervicogenic dizziness, that medical physicians do not have training or knowledge to refer out to us for this condition. Just recently, Reneker et al 2015 found a distinct difference between professions regarding utility of clinically diagnostic tests for differentiating cervical and other causes of dizziness s/p concussion. In fact, three tests, 1) passive joint mobilization, 2) palpation of cervical musculature and 3) joint position error testing were shown to have high utility to diagnose cervicogenic dizziness by PTs (62%, 53% and 47% respectively), but NONE of these were selected by a single neuro-otologist!
There is controversy between professions.
With such discrepancies between the philosophies and clinical approaches between the medical trades, it is no wonder there is never “cervicogenic dizziness / cervical vertigo” is not on a script. We must meet on the same playing field here and see both sides of the argument with the manual and non-manual fields.
TA fair result can only be obtained only by fully stating and balancing the facts and arguments on both sides of each question.
Charles Darwin
It can be challenging to go speak to physicians about this condition as we do not have the juice to provide in regards to evidence. However, this is an emerging area of practice and the physical therapy field is gaining traction in RCTs by Susan Reid’s work to put more power to our trade. With that being said, if you want to learn the evidence to present to physicians, either in the elderly, s/p concussion, s/p whiplash or some other head/neck insult—we got you covered because there is controversy between professions.
Cervicogenic Dizziness Course
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the authors (husband–a manual therapist a wife—a vestibular specialist), teach a very unique course combining both the theory and practice of vestibular and manual principles in their 2-day course. Pertinent to this blog post, the 2nd day includes the “Physio Blend”, a multi-faceted physiotherapist approach to the management of Cervicogenic Dizziness, which includes treatments of the articular and non-articular system of manual therapy and the most updated sensorimotor exercise regimen.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for more information.
AUTHORS
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts